Nursing in Ontario is in a state of crisis.
In May 2022, WeRPN commissioned a study to examine the issues currently facing nursing professionals in the province. The findings prove what many of us already fear: that for most nurses in Ontario, working conditions are only getting worse.
The study, “The State of Nursing in Ontario: A 2022 Review,” was a follow-up to a December 2020 poll and was conducted to compare present-day realities to nurses’ experiences at the height of the pandemic. A total of 762 RPNs were surveyed across all sectors, including Long-Term Care and Home and Community Care.
It’s well known that the COVID-19 pandemic has been one of the most challenging events for healthcare providers; staff shortages, burnout and pay stagnation crumbled an already taxed workforce.
And yet, even though the pandemic began over two years ago, these issues have not been resolved.
The findings of WeRPN’s study are alarming, and the public is starting to take note, with local and national media coverage via The Globe and Mail, Global Toronto, CTV News and City News.
Despite many aspects of life returning to a pre-pandemic normal, nursing professionals remain under-supported and overworked— a startling reality which will directly impact the provision of healthcare in Ontario.
It already has. In an interview with WeRPN’s CEO, Dianne Martin, City News reported that some Toronto intensive care units (ICU) are either at capacity or so understaffed that they cannot keep all beds in operation.
WeRPN is urging government leaders and policymakers to take action. “If we don’t start to solve the problem yesterday,” said Martin, “patients who are critically ill…we are going to lose some people.”
The report’s key findings are broken down as follows:
Unsafe workloads have become the new normal, and it’s impacting patient care.
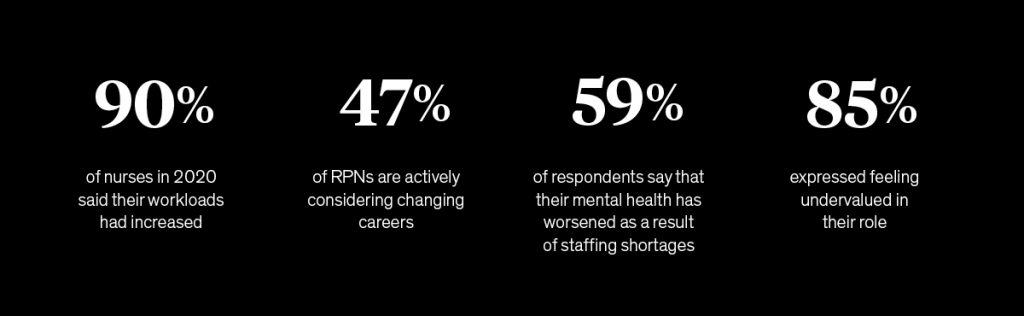
According to WeRPN, 90 per cent of nurses in 2020 said their workloads had increased due to the COVID-19 pandemic. But this trend hasn’t flatlined. Today, 93 per cent agree that their workloads have continued to increase over the last two years.
Alarmingly, 68 per cent of surveyed nurses reported that they do not have the time or resources available to provide adequate care to their patients, and 4 out of 5 have experienced moral distress due to their job. Many are now required to perform duties outside their scope of practice, actions they feel unprepared and unequipped to perform.
The consequences of unsafe workloads must not be over-looked: nurses are experiencing rising levels of distress and, despite their best efforts, patient care is being compromised.
Working conditions continue to worsen.
The vast majority of RPNs have been directly impacted by staff shortages, which has increased their job-related stress and led many to work unpaid overtime hours.
As quoted in the survey, one RPN stated, “The expectation is to do more than is humanly possible, throughout the shift, for every shift. And I constantly feel pressure to stay longer hours, with the guilt of not supporting the team if you don’t pitch in to do more, working through breaks, starting early and leaving late, and not being compensated for that. There is an overall lack of understanding and respect for an RPN’s work.”
This distressing trend led 59 per cent of respondents to say that their mental health has worsened as a result of staffing shortages.
A staggering number of RPNs are leaving the profession.
Ontario is at risk of losing almost half of its nursing professionals. According to the survey, 47 per cent of RPNs are actively considering changing careers, and 59 per cent of those plan to leave the healthcare sector altogether. RPNs are critical to our healthcare system, but current wages, workloads, unfair compensation practices and unsafe environments make many reconsider their postings.
As one RPN expressed, “honestly, no one should be surprised that RPNs are leaving. It is not worth the pay for so much work that never ends. And this job could not only make me sick but potentially also my family.”
Morale is low and dissatisfaction is high; nursing is now taking a personal toll.
In 2022, only 36 per cent of respondents felt supported in their jobs, compared to 67 per cent just two years earlier. This lack of support is manifesting in low job satisfaction and burnout. Nurses feel emotionally drained and unable to effectively support patients as a result.
As a healthcare worker, the stakes are always high. The consequences can be devastating if nurses do not have the appropriate financial, practical and emotional support. As one RPN describes, “when considering RPN pay, think about what human life is worth. Good care—that is what the pay should reflect. It should reflect those values. I medicate more than 40 patients. One error can kill someone. Extreme precision, knowledge, energy and alertness are needed. You must not be tired, sad or unfocused.”
Nurses are reaching their breaking point.
A shocking 94 per cent of nurses feel that their daily experiences at work have become significantly more stressful in the last two years. Part of this increased anxiety is related to financial stress—75 per cent of nurses in 2022 are experiencing financial hardship, with 62 per cent seeking extra shifts, 54 per cent working overtime and 43 per cent working a second job just to make ends meet.
This stunning under-appreciation and inadequate compensation is impacting RPNs’ mental health. Some no longer feel nursing is a sustainable career option. As one respondent said, “There is a lack of nursing staff, lack of support from management, lack of basic supplies (I was providing my own out of pocket). No vacation or time off, poor access to COVID-19 testing, miscommunication between facilities, inappropriate patients being admitted and no raise despite workload increase.”
RPNs are experiencing wage stagnation.
In April 2022, the Ontario government announced permanent wage increases for personal support workers (PSWs). RPNs supported this increase, but many were surprised that other health workers would not experience similar raises.
Though their role is closer to that of a Registered Nurse (RN), RPNs are now paid similar wages to PSWs. Some—in fact, 15 per cent of respondents—are currently managing PSWs earning more than them.
Despite higher workloads and less support, this wage stagnation has left many RPNs feeling unfairly compensated. And this issue is not only financial—85 per cent expressed feeling undervalued in their role.
One RPN clearly expressed this frustration: “I want to be recognized for what we do in our role. I am a surgical nurse and work to full scope. I am doing a job closer to an RN role than a PSW. I was a PSW for 20 years and went back to school to get a better education and earn more money per hour. Now I am making the same as a PSW. I agree PSWs should be paid more, but so should RPNs.”
Government leaders must focus on Ontario’s Long-term Care Sector.
As in other sectors, RPNs working in long-term care are overwhelmingly dissatisfied with their work and considering leaving the profession. Strikingly, 39% of nurses in this sector have said that workplace violence contributes to job dissatisfaction. These are unsafe and unsustainable working conditions that leaders must address.
WeRPN’s Calls to Action:
This study illuminates some of the critical issues facing the nursing profession today. In the aftermath of the global pandemic, nurses are being unfairly compensated, poorly supported, and as a result, compelled to leave.
WeRPN has released three main calls to action for government leaders and policymakers.
1. Repeal Bill 124 and increase RPNs wages.
WeRPN estimates that RPNs wages must be increased by at least 20% to be proportional to other nursing groups. Though long-term strategies will be necessary to address staffing shortages, increasing wages could improve RPN retention and provide a much-needed boost to morale.
2. Counteract the ongoing normalization of unsafe workloads.
This issue has become urgent and must be addressed. Leadership must acknowledge the unsafe workloads, the unfair expectations placed on nurses, and the consequences their patients face as a result. WeRPN recommends more full-time positions for RPNs and environments where nursing professionals feel safe and heard. At a minimum, RPNs should be able to take their entitled rest and breaks.
3. Include RPNs voices in policy making.
RPNs have a unique perspective that must be heard when envisioning new policies for the nursing profession. Their first-hand experience and expertise should be used as a resource.
As advocates for RPNs across Ontario, WeRPN is raising the alarm over worsening conditions in the nursing profession. Unsurprisingly, workloads soared, and stress increased during the global pandemic, but these realities are becoming a new normal that cannot be maintained.
Leaders must prioritize nurses’ safety and well-being to revitalize the healthcare sector and protect Ontarians.
